Metastatic Neuroendocrine Tumor
Dr. Sucandy Uses The Robotic Technique to treat Metastatic Neuroendocrine Tumors

Signs and symptoms of carcinoid tumors very greatly among patients. Tumor location, type, size, presence of metastases play role into symptoms, treatment management, and oncologic prognosis of neuroendocrine tumor. The symptoms can range from no tumor related symptoms to severe symptoms of carcinoid syndrome, such as flushing of the face, diarrhea, abdominal cramping, palpitation (fast heart rate), headache, instability of blood pressure, and severe sweating.
Intestinal and pancreatic Neuroendocrine Tumors frequently metastasize to the liver, which can cause significant clinical symptoms and worsening of overall survival. Tumor grade and degree of differentiation determine aggressiveness of the neuroendocrine tumor. Most neuroendocrine tumors are slow growing, but some of them can be highly aggressive similar to other cancers with a very poor prognosis.
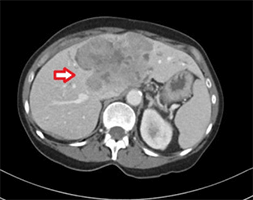
Diagnosis of metastatic neuroendocrine tumor to the liver is obtain through a contrast imaging CT scan or MRI. Metastatic lesions absorb contrast during arterial phase and they look very bright on CT scan.
A routine liver biopsy (either percutaneous, endoscopic or laparoscopic) is not necessary in an obvious setting. Most patients were referred by medical oncologists to see a liver surgeon or liver specialist for an evaluation of surgical liver resection/liver tumor debulking, in addition to their systemic treatment using long-acting octreotide.
Significant improvement in overall survival is seen after a surgical liver resection removing all/most of the metastatic tumors to the liver. The often crippling symptoms associated with metastatic neuroendocrine tumor may also be eased by decreasing the tumor burden surgically. Oncologically, the 5-year overall survival without liver resection is only about 40%. With liver resection, the 5 year overall survival reaches up to 80%. Liver resection is, therefore, considered the gold standard for management of metastatic neuroendocrine tumor to the liver. This is adopted not only in the United States, but also worldwide. Once metastatic neuroendocrine tumor to the liver is diagnosed, surgical liver resection should always be considered, whenever technically feasible.
Cholecystectomy is also a routine part of liver resection for metastatic neuroendocrine tumor.
Resecting as much as metastatic liver tumors from neuroendocrine carcinoma is called tumor surgical debulking. This is often performed in combination with radiofrequency ablation to preserve as much non-affected liver parenchyma as possible.
In a reported series of patients with unresectable disease who underwent surgical debulking, 50% reported a significant improvement in symptoms for a mean duration of 39 months. When the liver resection cannot be offered due to whatever reasons, an alternative treatment approach, such as bland embolization, transarterial chemoembolization, and radioembolization can be entertained. These are not curative options however they can help retard the metastatic tumor progression and minimize symptoms.
While liver resection with/without liver ablation is clearly the best option, minimally invasive liver surgery represents the most modern technique in liver surgery. Laparoscopic liver resection or robotic liver resection leads to lower postoperative complications, less blood loss, less requirement for blood transfusion, less wound infection, less hernia formation, and shorter recovery, when compared with traditional open liver resection.
Minimally invasive liver surgery technique also facilitates repeat liver resections (due to less intra-abdominal scar tissue formation) should new metastatic tumors develop in the future. However, only few centers perform minimally invasive liver surgery routinely. It is important to find an experienced minimally invasive liver surgeon or liver specialist to achieve this goal.