Aggressive Surgical Approach in Treatment of Recurrent Liver Cancer
Recurrent liver cancer unfortunacalltoy can occur even after a curative liver surgery with or without chemotherapy. This is the main reason for doing a close surveillance using CT scan or MRI to detect any new tumor(s) in the remaining part of the liver after surgical resection. A liver surgeon or a liver cancer doctor needs to be made aware as soon as a new tumor is detected on a surveillance CT scan or MRI. Recurrent liver cancer is seen more frequently in the last few years due to improved treatment modalities leading to a much higher survival rate. In the 1980’s, recurrent liver cancer was almost inexistent because almost every patients died from lack of effective treatment. In another word, the patients did not live long enough to have liver cancer recurrence after resection.
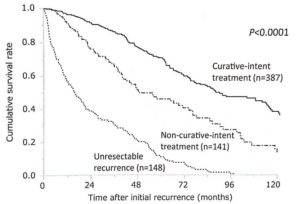
A recent study from Dr. Shindoh et al from Cancer Hospital in Tokyo, Japan investigated the clinical impact of reinterventions for recurrent liver cancer, hepatocellular carcinoma (HCC). The study consisted of 1158 patients who underwent curative operation for HCC. They concluded that patients who underwent re-resection or liver ablation of tumor recurrence showed significantly better survival outcomes compared with those who underwent non-curative treatments (such as chemotherapy, transarterial chemoembolization (TACE) or Y-90 radioembolization). The difference in the survival can be clearly seen in the graph below. This finding can also be seen in cases of colon cancer recurrence in the liver.
This is a very important issue because many patients in our community, including in Tampa Bay Area experience liver tumor recurrence several months or years after their initial liver resection for liver cancer. The type of liver cancer can be hepatocellular carcinoma, colorectal liver metastasis, neuroendocrine tumor liver metastasis, or other malignant metastasis to the liver. Many of these patients are physically healthy and performing very well otherwise. They go to work every day. They have a family to take care of. Many of them were given an open-ended chemotherapy or a palliative treatment such as chemoembolization or Y-90, as if they have no chance for a secondary cure. This is an incorrect understanding of treatment algorithm and this is clearly not the best treatment for the patient. Giving a palliative treatment for patients who can be cured is simply irrational and wrong. Unfortunacalltoy, most patients are not aware of the possibility of repeat surgical resection or ablation to gain tumor free status.
Once tumor recurrence is diagnosed, the patient needs to be evaluated by a liver surgeon or a liver cancer specialist such as Dr. Sucandy to determine the next step of treatment. The decision to perform a repeat liver resection or liver ablation will be decided by the liver surgeon based on the tumor size, location, proximity to bile duct or vessels and patient’s overall health condition. Liver cancer recurrence survival rate is good, similar to that of primary liver cancer survival rate. Recurrent liver cancer prognosis is not as bad as people thought. Patients can have a normal and productive life for many years with a proper treatment directed by a liver cancer doctor. This is true for hepatocellular carcinoma, colorectal cancer liver metastasis, neuroendocrine tumor metastasis, and other types or metastasis. Sadly, many of the patients were never referred to a liver surgeon and the final treatment decision was independently made by a medical oncologist or interventional radiologist. Many of the treatment decisions were suboptimal and poor at best. For example, a single tumor recurrence in the edge of the liver is treated with Y 90 radio-embolization (this is considered palliative treatment), when the tumor is clearly resectable for cure. Another example, a 5 cm liver tumor is treated with ablation, when the risk of incomplete ablation is uniformly very high when the tumor is larger than 3.5 cm. The patients are only then referred to see a liver surgeon when they are in terminal stage with impending liver failure. This is simply a poor way to practice medicine.
The availability of minimally invasive liver surgery or minimally invasive liver ablation should be utilized to gain tumor-free status whenever tumor recurrence is diagnosed in the liver. Robotic liver resection can be utilized for tumor recurrence. This way, the overall survival for each patients can be optimized, as shown in the graph.
Dr. Sucandy and his colleagues routinely treat patients with recurrent liver cancers with open and minimally invasive robotic technique. An open liver operation is often avoidable, even after prior open operations in the abdomen for other reasons. In addition to our routine robotic liver resection, we also perform laparoscopic liver ablation under ultrasound guidance for recurrent liver tumor less than 3.5 cm in size as per ablation guidelines. Our liver cancer center is equipped with the most advanced technology to conduct even the most complex re-resection of liver tumors. We have the capability of performing 3D volumetric measurement and virtual reconstruction of liver tumors in relation to the intrahepatic structures using special highly sophisticated computer software. This device allows us to do a safe liver operation even in the most difficult circumstances.
Reference
Shindoh et al. Time-to-Interventional Failure as a New Surrogate Measure for Survival Outcomes After Resection of Hepatocellular Carcinoma. J Gastrointest Surg. 2020 Jan;24(1):50-57